It’s easy to mistake Kawasaki disease for just another childhood disease that will pass with time, especially since it has a common symptom like fever. But unlike typical fevers, Kawasaki disease brings with it a high risk of complications. In fact, it is a leading cause of heart disease during childhood which affects children under 5 years old. Kawasaki disease, though, is not contagious, nor is it widely understood by most parents, which can make the symptoms go to be overlooked.
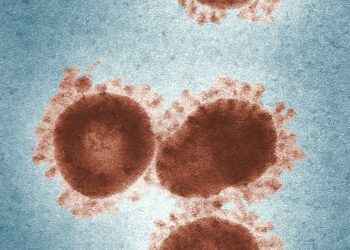
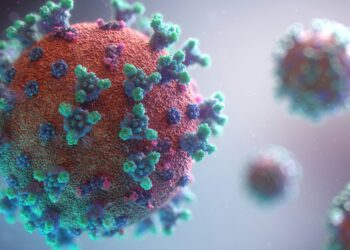
Kawasaki Virus is a virus that causes the blood vessels to swell throughout the body, most especially the coronary arteries, which are responsible for supplying blood to the heart. Because its exact cause is still unknown, parents often misinterpret its signs and eventually delay medical attention which can be very life-threatening for the child. Let us look at ways to diagnose and treat Kawasaki disease.

Diagnosing Kawasaki Disease
You are probably wondering how doctors diagnose this disease if its symptoms look just like any other common illness.
First of all, the doctor looks at a combination of signs and then he conducts certain tests to confirm the diagnosis. There are specific diagnostic criteria to decide if a child might have Kawasaki Disease.
The “five symptoms” the doctors look for usually last for several days. This includes a fever which lasts for at least five days. Typically, a Kawasaki Disease fever is higher than 101°F or 38.3°C, a rash on the body, swelling of the hands and feet, bloodshot eyes without any discharge that looks like that of conjunctivitis, a strawberry tongue and swollen lymph nodes.
If a child has most of these symptoms, the doctor would suspect Kawasaki Disease. But this is not enough evidence to diagnose a child with Kawasaki Disease. The doctor would then proceed to order some blood tests, which would allow him to look for signs like swelling or infections in the body. The most common tests for Kawasaki disease include:
Complete Blood Count (CBC): CBC checks the number of different types of blood cells. It shows if the body is fighting an infection or if there is a lot of swelling in the body.
C-reactive Protein (CRP): When the body is inflamed, it produces C-reactive protein. High levels of C-reactive protein in the blood shows that something in the body is causing inflammation.
Erythrocyte Sedimentation Rate (ESR): The ESR test measures how quickly red blood cells settle at the bottom of a test tube. A faster than normal rate shows inflammation in the body.
Treatment of Kawasaki
The next step after diagnosing Kawasaki disease is to begin treatment. This treatment is to reduce swelling and prevent any serious heart issues from occurring.
Primary Treatment: The primary treatment for Kawasaki disease is intravenous immunoglobulin, (IVIG). IVIG is a special treatment that involves giving the child immunoglobulin, which is a kind of antibody, through a vein. IVIG helps reduce the swelling in the blood vessels and lowers the risk of heart damage, especially in the coronary arteries. It’s mostly effective when given within the first 10 days of the illness.
Aspirin: Doctors also use aspirin to treat Kawasaki disease. Aspirin helps in two ways: a high dose of aspirin is given to help lower the fever and then reduce swelling throughout the body. While a low dose aspirin is continued after the fever goes away. This is to prevent blood clots. Blood clots are risked because of the damage and swelling in the arteries.
Supportive Care: In addition to IVIG and aspirin, doctors often provide supportive care to help the child feel more comfortable during recovery. This includes giving medication like acetaminophen (tylenol) or ibuprofen to lower the fever and help with the discomfort.
The doctor also makes sure that the child is well hydrated, especially since they may have lost a lot of fluids during the fever. This fluid can be given by mouth or sometimes through an IV. Lastly, if the child is feeling pain from the swelling, they may be given additional medication to ease their pain.
Final Note: What Happens After Treatment?
Typically, after treatment, most children will fully recover. However, some children may need follow-up care to monitor their heart health, particularly if the swelling affected their coronary arteries. The doctor may also do heart tests like an echocardiogram to check for any long-term damage to the heart.